Table of Contents
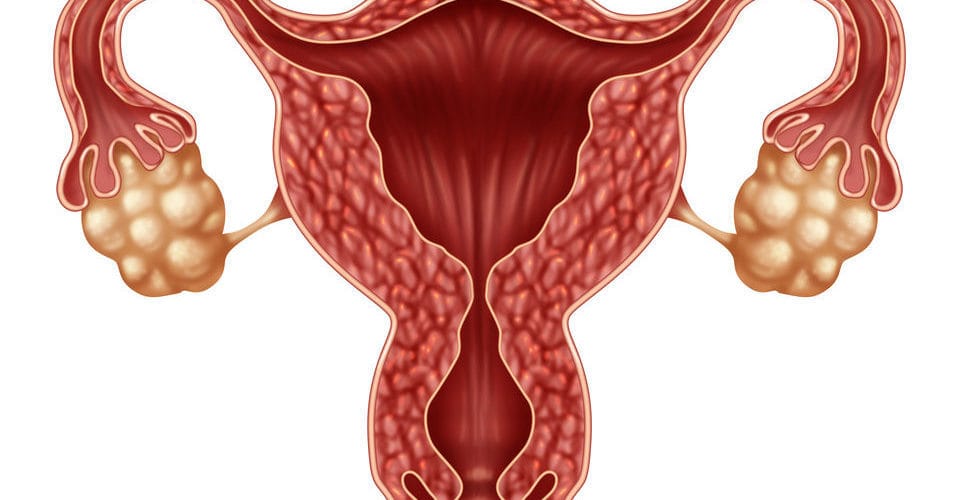
Ovarian cysts are fluid-filled sacs that develop on or within an ovary. They’re common across all ages but especially prevalent during childbearing years. Most cysts are harmless and resolve without treatment. However, some can cause symptoms or complications requiring medical attention. Understanding the types, symptoms, diagnosis, and treatment options can help you manage ovarian cysts effectively.
Types of Ovarian Cysts
- Functional Cysts
- Follicular Cysts: During a normal menstrual cycle, an egg develops inside a follicle. If the follicle doesn’t release the egg, it can continue growing into a cyst.
- Corpus Luteum Cysts: After ovulation, the empty follicle (corpus luteum) normally breaks down. If it seals off and fills with fluid, a cyst forms.
- Pathological (Neoplastic) Cysts
- Dermoid Cysts (Mature Cystic Teratomas): Contain various tissues—hair, fat, or teeth—derived from germ cells.
- Cystadenomas: Develop from ovarian surface cells and may be filled with a watery or mucous material.
- Endometriomas (“Chocolate Cysts”): Form in women with endometriosis when uterine-lining tissue grows on the ovaries.
- Polycystic Ovary Syndrome (PCOS)
A hormonal disorder characterized by multiple small follicles (cysts) and symptoms like irregular periods, excess androgen, and insulin resistance.
Common Symptoms
Many ovarian cysts are asymptomatic and discovered incidentally during routine exams. When symptoms do occur, they may include:
- Pelvic Pain: Dull or sharp ache on one side, often during ovulation or menstrual bleeding.
- Bloating or Abdominal Fullness: Due to the cyst’s size or pressure on surrounding organs.
- Pain During Intercourse: Deep pain or discomfort when the cyst is disturbed.
- Frequent Urination: Cysts pressing on the bladder reduce its capacity.
- Menstrual Irregularities: Heavy, light, or irregular bleeding.
- Nausea or Vomiting: Particularly if a cyst ruptures or causes ovarian torsion (twisting).
If you experience sudden, severe pelvic pain, fever, dizziness, or rapid breathing, seek immediate medical care—it could indicate a ruptured cyst or torsion, both of which are medical emergencies.
Risk Factors
While anyone with ovaries can develop a cyst, certain factors increase the likelihood:
- Hormonal Issues: Fertility treatments that stimulate ovulation can promote cyst formation.
- Endometriosis: Raises the risk of endometriomas.
- Pregnancy: Some cysts form early in pregnancy and usually disappear by the second trimester.
- Severe Pelvic Infections: Can spread to the ovaries and fallopian tubes, causing cysts.
- PCOS: Characterized by multiple ovarian follicles.
Diagnosis
Your healthcare provider will begin with a thorough history and pelvic exam. Diagnostic tools include:
- Ultrasound
Transvaginal or abdominal ultrasound images reveal cyst size, shape, and composition (solid vs. fluid-filled). - Blood Tests
- CA-125: Elevated levels may suggest a higher risk of malignancy in postmenopausal women, but many benign conditions also raise CA-125.
- Hormone Levels: To assess PCOS or other endocrine disorders.
- Additional Imaging
CT scans or MRI may be used if ultrasound findings are inconclusive. - Laparoscopy
A minimally invasive surgical procedure allowing direct visualization—and possibly biopsy—of the cyst.
Treatment Options
Treatment depends on cyst type, size, symptoms, and patient’s age or reproductive desires:
- Watchful Waiting
Functional cysts under 5 cm often resolve within one to three menstrual cycles. Follow-up ultrasounds monitor changes. - Hormonal Birth Control
Oral contraceptives or progestin therapy prevent ovulation, reducing the risk of new functional cysts. - Pain Management
Nonsteroidal anti-inflammatory drugs (NSAIDs) like ibuprofen can relieve menstrual and cyst-related discomfort. - Surgical Intervention
- Laparoscopy (“keyhole” surgery) for cysts larger than 5–10 cm, persistent or symptomatic cysts, or suspicious features.
- Laparotomy (open surgery) for very large or possibly malignant cysts. Ovarian-sparing techniques remove only the cyst, preserving fertility. In postmenopausal women or malignancy risk, oophorectomy (ovary removal) may be advised.
Preventing Recurrence
While not all cysts are preventable, you can take steps to minimize recurrence:
- Regular Gynecological Exams: Early detection of new cysts via pelvic exams and ultrasound.
- Manage Underlying Conditions: Control PCOS with diet, exercise, and medications such as metformin. Treat endometriosis symptoms to reduce endometrioma formation.
- Healthy Lifestyle: Maintain a balanced diet and regular exercise to support hormone balance.
Impact on Fertility
Most functional cysts don’t affect fertility and resolve on their own. However, conditions like large endometriomas or PCOS can impair ovulation or cause adhesions. Early diagnosis and tailored treatment—including fertility-preserving surgery or assisted reproductive techniques—help many women achieve successful pregnancies.
When to Seek Medical Advice
Contact your healthcare provider if you experience:
- Persistent or severe pelvic pain
- Noticeable abdominal swelling
- Unusual menstrual changes
- Symptoms of torsion or rupture (acute pain, fever, vomiting)
Conclusion
Ovarian cysts are a common gynecological issue, but with timely diagnosis and individualized care, most women can manage cysts effectively and maintain reproductive health. By understanding cyst types, recognizing warning signs, and partnering with a knowledgeable healthcare team, you can navigate treatment options confidently—preserving both your well-being and quality of life.